About Merit-based Incentive Payment System (MIPS)
In addition to serving multiple functions as the clinical data registry for otolaryngology-head and neck surgery, Reg-ent can also be utilized for MIPS reporting. Reg-ent is a CMS-designated Qualified Clinical Data Registry (QCDR) and accommodates reporting and submission for three MIPS 2023 performance categories: Quality, Promoting Interoperability, and Improvement activities. Participants can see visual representations score estimates, and guidance throughout the reporting and submission process. Reg-ent also offers feedback opportunities, such as trending their quality data over time and comparing performance to Reg-ent participants, clinicians within their practice, and national CMS Historical Benchmarks. For more on MIPS reporting requirements and available Reg-ent quality measures, click on the resource bars below.
Who is Eligible and/or Required to Participate Within MIPS?
The 2023 MIPS eligible clinician types are physicians (MD, DO, DDS, DMD, DPM, OD), osteopathic practitioners, chiropractors, physician assistants, nurse practitioners, certified nurse anesthetists, physical therapists, occupational therapists, clinical psychologists, qualified speech-language pathologists, qualified audiologists, registered dietitians or nutrition professionals, clinical social workers, and certified nurse-midwives.
There are additional exclusions, such as:
- If initially enrolled in Medicare within the current performance year
- Clinician involved in an Advanced APM (Alternative Payment Models).
- The final check to determine MIPS eligibility is the volume of Medicare patients seen by the clinician. To exceed the low-volume threshold for the 2023 performance year, a clinician must:
- Bill more than $90,000 for Part B covered professional services under the Physician Fee Schedule (PFS), and
- Provide services to more than 200 Medicare Part B patients, and
- Furnish more than 200 covered professional services to Part B Medicare Patients.
If the eligible clinician type or group meets some (but not all) of the low volume thresholds and are not included in an eligible group submission, they are not required to report MIPS. However, they can elect to submit as a:
- Voluntary Reporter: Excluded and will not receive a MIPS payment adjustment
- Opt-In Reporter: If the exclusion criteria is the low-volume threshold was not achieved, a clinician may choose to participate and would be eligible to receive a payment adjustment.
For more information on MIPS eligibility, please review the Eligibility and Participation Quick Start Guide.
CMS has provided a visual aid to determine clinician eligibility, click to download:
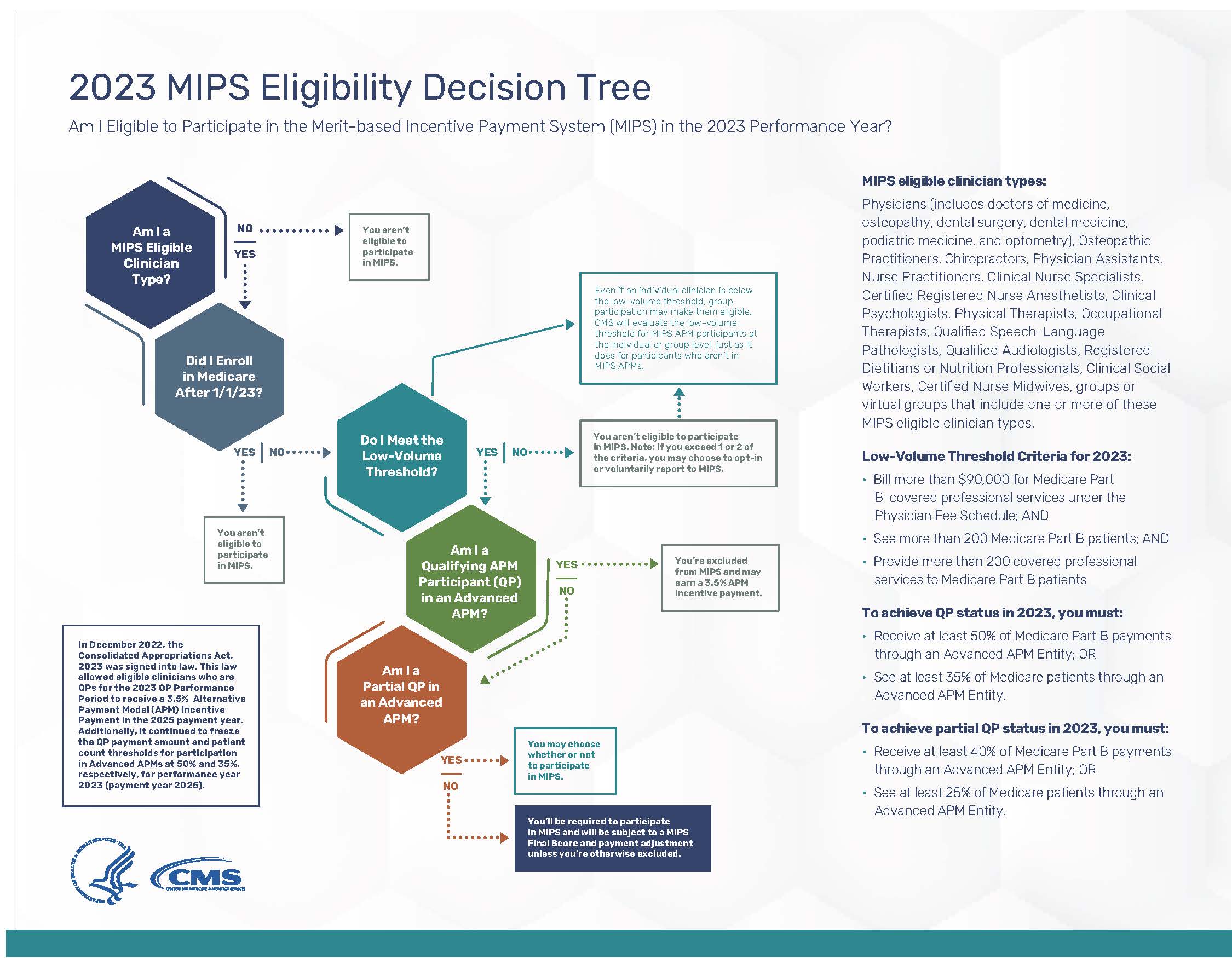
To check your Eligibility Status, visit the QPP Participation Status webpage.
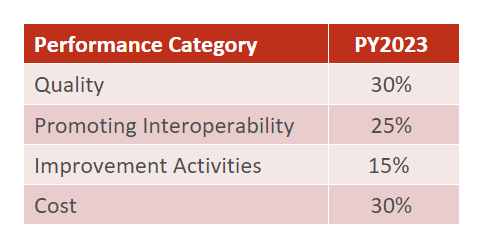
How will Clinicians Be Scored?
To be eligible for a positive payment adjustment, a reporting clinician or group must meet the performance threshold and earn at least 75 points. The final MIPS score will be calculated based on the following weights across four performance categories, if no category exclusions or exceptions are approved:
- 2023 Quality Quick Start Guide
- 2023 MIPS Promoting Interoperability User Guide
- 2023 MIPS Improvement Activities User Guide
- 2023 MIPS Cost User Guide
Estimates will be available for quality, improvement activities, and Promoting Interoperability on your Reg-ent dashboard. The cost performance category is calculated by CMS after the performance year based on your Medicare claims for the year. For more information on MIPS Scoring, Coming soon, Reg-ent will provide once CMS releases the 2023 Traditional MIPS Scoring Guide.
How does MIPS impact my payment?
Payment adjustments are applied two years after the performance period. For example, the data submitted for PY2023 will determine the 2025 payment adjustment. Your final MIPS score will determine the adjustment. A Final Score Preview will be made available by CMS in June.
Tips for MIPS
- Communicate any plans to change electronic health records as early as possible
- Select meaningful Quality and Improvement Activity measures
- Review quality measure benchmarks to maximize points
- Review opportunities for bonus points among Promoting Interoperability measures
- Review your clinician and location list for completeness and accuracy
- Review all submitted performance categories
Frequently Asked Questions about MIPS
1. How do Reg-ent participants submit to MIPS?
Each February/March, Reg-ent participants will receive an email notification that the MIPS Submission Module is open for the previous performance year. Practices are encouraged to schedule a time to submit their performance data to CMS. Reg-ent will provide a checklist of steps to complete prior to the call for seamless submission.
2. What quality measures are required to report?
In 2022, there are no specific quality measures required. Practices must select at least six quality measures, including one outcome measure or a high-priority measure. We encourage practices to report all operational measures including Academy-developed AAO measures. CMS can establish performance period benchmarks when at least 20 instances of the measure are reported through the same collection type and meet data completeness and case minimum requirements and have a performance rate greater than 0% (or less than 100% for inverse measures). CMS takes the highest scoring measures into consideration when determining Quality score. Review the Reg-ent quality measure by visiting the AAO-HNSF Endorsed Measures webpage.
3. What is required for satisfying the improvement activity performance category?
Practices are required to implement 2 to 4 improvement activities to receive the maximum score of 40 points. Each improvement activity is worth 10 to 40 points depending on its weight (medium or high) and applicable special status designations. Medium-weighted activities are worth 10 points and high weighted activities are worth 20 points. For clinicians and groups with certain special status designations (small practice, non-patient facing, rural, or Health Professional Shortage Area (HPSA), points double to 20 for medium-weighted and 40 points for high-weighted improvement activities.
Most improvement activities have a performance period of 90 continuous days for most improvement activities with a few exceptions. Practices are required to attest to activities during submission and do not have to submit any supporting data, but practices must keep documentation of the efforts to meet the improvement activity for 6 years subsequent to submission. For a full list and validation requirements for each improvement activity, download: 2023 MIPS Data Validation – Improvement Activities Performance Category Criteria.
4. What is required for Promoting Interoperability?
Practices are required to submit collected data for certain measures from each of the four objectives measures (unless an exclusion is claimed) for the same 90 continuous days (or more) using Certified EHR Technology (CEHRT). New for 2023, in addition to requiring a yes/no response for the required Public Health and Clinical Data Exchange measures, the measure requires MIPS eligible clinicians to submit their level of active engagement. Some measures within this performance category that can be excluded if they do not apply to your practice.
5. What happens if a clinician or group cannot complete one of the performance categories?
In some cases, a performance category will be reweighted to 0% of the total score. This typically requires CMS approval for an exception or exclusion. In these cases, the points from the excluded categories are reassigned to another category. This distribution depends on the number and type of performance categories submitted.
Are you a small practice?
We recommend signing up for CMS’s QPP Small Practices Newsletter.
