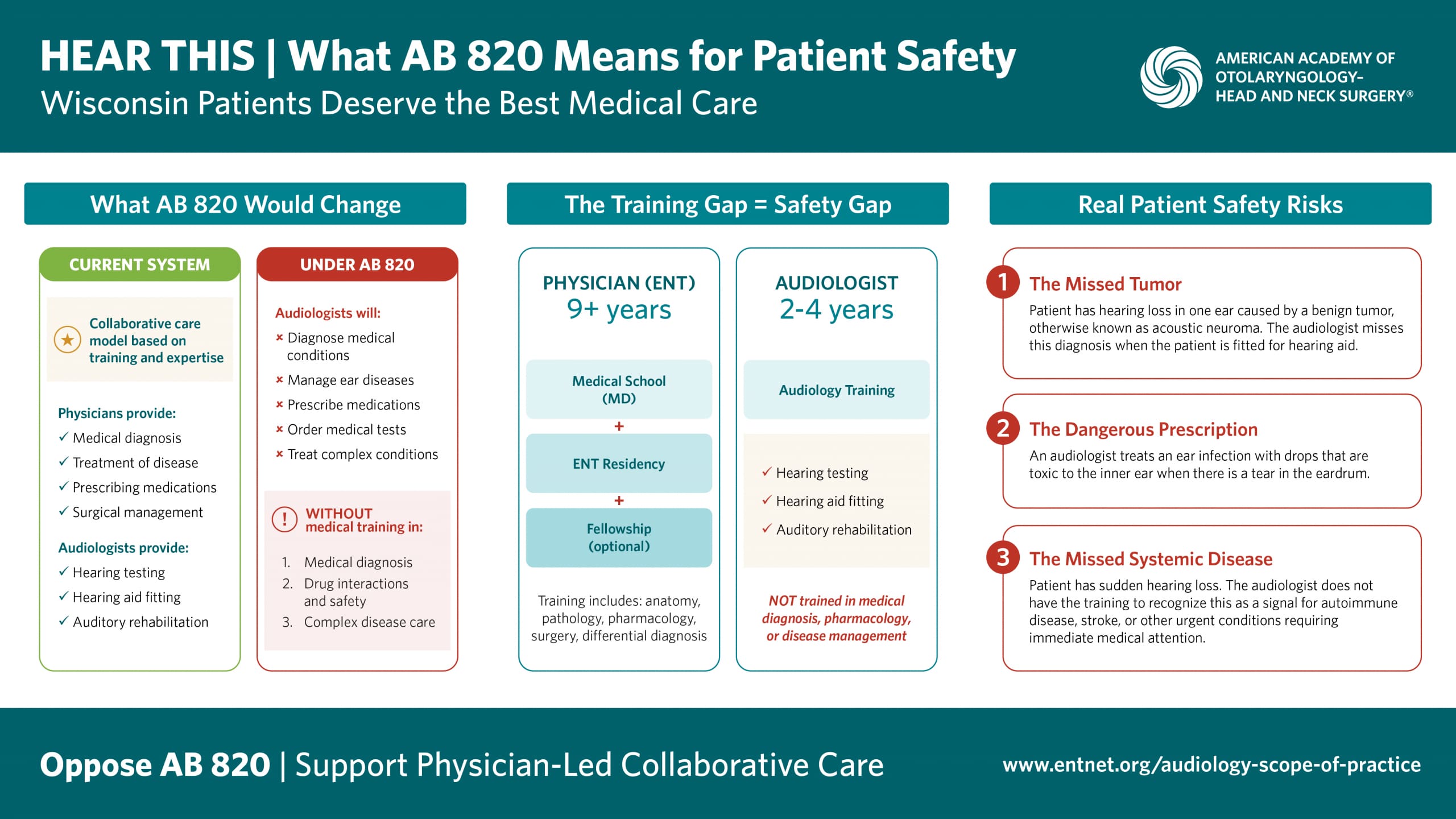
The American Academy of Otolaryngology–Head and Neck Surgery (AAO-HNS) strongly opposes legislative efforts to expand the scope of practice for audiologists beyond their level of training. This includes expansion into areas of medical diagnosis and treatment. While audiologists are valued members of the hearing healthcare team, their training does not prepare them to perform medical procedures, order and interpret diagnostic tests, prescribe medications, or manage systemic disease. Such expansions would endanger patient safety, increase healthcare costs, and fragment care.
We Share the Goal, Not the Method
Otolaryngologists and audiologists both want the same thing: patients getting excellent, timely hearing healthcare. We work side-by-side every day because audiologists are important members of the hearing healthcare team. However, wanting to improve access doesn’t mean we should bypass the safety guardrails that protect patients. We shouldn’t have to choose between quick access and safe care. Scope expansion legislation presents a false choice. It claims we must sacrifice physician oversight to improve access. All patients deserve both timely care and proper diagnosis and treatment.
The Training Gap Creates a Safety Gap
Patient safety and diagnostic accuracy must be the foundation of any scope-of-practice decision. Scope expansion asks audiologists to practice beyond their training into medical diagnosis, pharmacology, surgical principles, and systemic disease management.
Real Risks to Patients
We surveyed practicing otolaryngologists across the country about scope expansion efforts. These are their real concerns:
The Missed Diagnosis Problem: Hearing loss is a medical condition that requires medical evaluation. Physician-led care ensures patients receive the correct diagnosis and the appropriate care. A 55-year-old with hearing loss in one ear might receive testing and a hearing aid from an audiologist, but a physician knows to order an MRI first, because unilateral hearing loss can be the first sign of an acoustic tumor or cyst. Catching that early could save the patient’s facial nerve, their balance, even their life.
“Audiologists have missed cholesteatomas that have grown under their care when not referred to an otolaryngologist.” — Practicing Otolaryngologist, West Virginia
“I have seen patients where an audiologist documented a normal eardrum, when the patient actually had an infection or cholesteatoma.” — Practicing Otolaryngologist, Michigan
“Lack of recognition of underlying pathology associated with unilateral effusion or hearing loss may delay diagnosis of head and neck cancer.” — Practicing Otolaryngologist, Nevada
Procedure Complications: Procedures such as cerumen removal and foreign body extraction carry risks including canal trauma, eardrum perforation, and infection requiring surgery.
“When audiologists have removed wax, multiple times they have done an incomplete job or ignored the wax on the tympanic membrane, which is hard to get.” — Practicing Otolaryngologist, West Virginia
“Audiologists, without adequate training, can cause serious harm including eardrum perforation or hearing loss when removing a foreign body.” — Practicing Otolaryngologist, Arkansas
Improper Testing and Follow-Up: Audiologists lack training to select or interpret radiologic studies and laboratory tests. A patient with pulsatile tinnitus may need specific vascular imaging. Ordering the wrong scan or test misses critical diagnoses. Sudden hearing loss requires urgent medical evaluation and the appropriate tests need to be conducted as soon as possible.
“Audiologists should not be ordering any kind of radiology or functional tests. This is beyond their scope of practice.” — Practicing Otolaryngologist, Maryland
“If audiologists are granted the ability to order bloodwork and radiologic scans, there is a risk of overuse, misinterpretation, and increased cost of care.” — Practicing Otolaryngologist, Arizona
The Wrong Medication: Audiologists are not trained in any way to order prescription medication. The effective use of prescription medication requires proper diagnosis by a physician. Only physicians are trained to recognize what medications are appropriate and when they should not be administered. As an example, an audiologist may prescribe antibiotic drops to a patient with an ear infection. However, if their eardrum is perforated, some drops are toxic to the inner ear and could cause permanent hearing loss. A physician examines the eardrum before prescribing. That’s a detail that requires medical training.
“I have had to perform surgery to remove material an audiologist squirted into the patients ear canal without seeing that the patient had a hole in their eardrum.” — Practicing Otolaryngologist, Washington
This Does Not Solve Access Problems: Expanding scope does not address workforce shortages, even in rural areas. Both otolaryngology and audiology are experiencing shortages across the country. However, audiologists do not practice in rural areas at higher rates than physicians and they do not adequately replace physician-led care. Audiologists serve a specific role in the hearing healthcare team. Burdening them with medical responsibilities they are not trained for reduces the excellent hearing care they currently provide.
“There is an extreme shortage of audiologists across the country. Expanding their scope will only overburden them further and worsen care in rural areas.” — Practicing Otolaryngologist, Maryland
If we truly want to improve access to hearing healthcare, let’s talk about solutions that actually work:
- Telemedicine consultations for rural patients
- Collaborative care protocols where audiologists and physicians work together efficiently
- Streamlined referral pathways with clear criteria
- Training more otolaryngologists and audiologists
These approaches improve access without compromising the physician oversight that protects patients from misdiagnosis and delayed care.
Protecting Partnership, Not Territory
Walk into any ENT practice and you’ll find otolaryngologists and audiologists working together seamlessly. We rely on our audiology colleagues every single day for sophisticated hearing tests, hearing aid fitting and programming, and rehabilitation services. That partnership works because everyone operates within their scope of training. Scope expansion would disrupt this successful collaboration by asking audiologists to step into roles they’re not trained for—putting them in impossible positions with medical decisions and liability beyond their preparation. We don’t want that for our audiology colleagues, and we certainly don’t want it for patients.
The Bottom Line
- Faster access to the wrong diagnosis or improper treatment does not help patients.
- Training matters. Experience matters. Shortcuts create risks.
- Scope-of-practice legislation asks audiologists to exceed their training.
- States can improve access while maintaining safety—we don’t have to choose.
AAO-HNS urges policymakers to reject legislation that would improperly expand audiology scope of practice and put patient safety at risk. Instead, work with us on real solutions: telemedicine, enhanced collaboration protocols, and adequate workforce development. These approaches improve access without compromising patient safety.