Our Position
Congress must take action to reform existing administrative hurdles that limit access to prompt patient care by passing the Safe Step Act (S. 652/ H.R. 2630) and the Improving Seniors’ Timely Access to Care Act of 2023.
The Safe Step Act would create an expedient and medically reasonable step therapy exceptions process whereby patients could receive timely and necessary care without experiencing unnecessary delays and burdensome administrative hurdles to treatment. Additionally, the Improving Seniors’ Timely Access to Care Act of 2023 would create a streamlined and standardized prior authorization (PA) process that would remove unnecessary barriers to care and relieve the administrative burden shouldered by physicians – a factor that contributes to high rates of physician burnout and stress and ultimately, limits a physician’s ability to provide timely care to patients.
Background
Prior authorization is a process whereby physicians must obtain approval from a patient’s health insurer before providing care, to ensure that the service is covered by the patient’s health insurance plan. This requirement creates a significant burden for physicians and their patient care team which can delay the time necessary for diagnosis and treatment – potentially putting the health of the patient at risk.
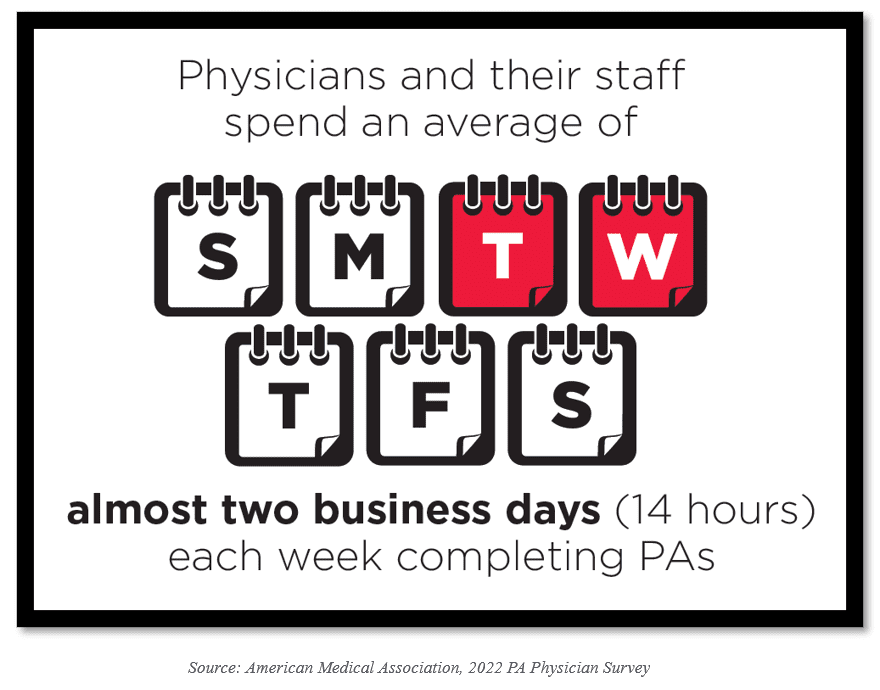
In the practice of otolaryngology, ENT offices currently complete an average of over 40 prior authorizations each week, and many offices have staff dedicated solely to the completion of prior authorizations each week. To compound this issue, many basic ENT procedures now have a prior authorization requirement and the requirements outlined for each prior authorization varies from health insurer to health insurer. The ensuing result is a patchwork system that is increasingly complex and creates an administrative burden for medical practices that exacerbates delays in patient care and contributes to rising levels of physician burnout and stress.
Another process that physicians must undertake to obtain the necessary treatment for their patients is seeking approval from a health insurer or pharmacy benefit manager (PBM) to cover the cost of a recommended drug, when lower-cost drugs are available. Medication step-therapy protocols, and more broadly utilization management programs, create significant barriers for patients by delaying the start or continuation of necessary medical treatment and potentially, contributing to prolonged and adverse patient care.
Congress can protect patients by reforming prior authorization
The Improving Seniors’ Timely Access to Care Act of 2023 would create sensible rules to relieve the administrative burden physicians face with prior authorization under the MA program. Insurers would be required to provide information on the care subject to PA, the average time PA approvals take, and the percentage of PA requests that are approved and denied.
This bipartisan legislation would also:
- Establish a PA program that provides real-time decisions in response to requests for items and services that are routinely provided
- Create a secure electronic PA (ePA) process and require MA plans to adopt ePA capabilities
- Ensure PA requests are reviewed by a qualified medical professional
- Increase transparency requirements by publishing specified PA information
- Ensure continuity of care when a patient transitions between MA plans
