Humanitarian medical efforts can be immensely rewarding and serve as a reminder to the motivation for choosing medicine as a career path. Travel grants provide residents who are Academy members an opportunity to contribute professional service to people in countries with limited resources. The deadline for grant applications for missions taking place July 1 – December 31, 2021, is May 31. Learn more.

In January 2020, a team of volunteers from Northwest Medical Volunteers and Face to Face traveled to Phnom Phen, Cambodia, to provide care to patients with congenital, traumatic, and neoplastic face deformities.
Jonnae Y. Ostrom, MD and Sarah R. Akkina, MD, MS
In January 2020, a team of volunteers from Northwest Medical Volunteers and Face to Face traveled to Phnom Phen, Cambodia, to provide care to patients with congenital, traumatic, and neoplastic face deformities. This mission has been ongoing since 2006 when it was started by Seattle otolaryngologist Craig S. Murakami, MD, and Cambodian plastic surgeon Theavy Mok, MD. Since then, groups of surgeons, anesthesiologists, nurses, and child life specialists have traveled to Cambodia annually to serve the Khmer people. The focus of these humanitarian missions is to provide care in the form of microtia repair, cleft lip and palate repair, complex facial reconstruction, and head and neck cancer surgeries that would otherwise not be available. During this specific mission, a record 149 patients were screened, which resulted in 11 microtia repairs and various other reconstructive surgeries over the course of a week.
with congenital, traumatic, and neoplastic face deformities. This mission has been ongoing since 2006 when it was started by Seattle otolaryngologist Craig S. Murakami, MD, and Cambodian plastic surgeon Theavy Mok, MD. Since then, groups of surgeons, anesthesiologists, nurses, and child life specialists have traveled to Cambodia annually to serve the Khmer people. The focus of these humanitarian missions is to provide care in the form of microtia repair, cleft lip and palate repair, complex facial reconstruction, and head and neck cancer surgeries that would otherwise not be available. During this specific mission, a record 149 patients were screened, which resulted in 11 microtia repairs and various other reconstructive surgeries over the course of a week.
In addition to helping patients who would otherwise not have access to such procedures, volunteers work closely with local physicians and residents from the Cambodian medical schools. After the reign of the Khmer Rouge ended in 1979, only 29 physicians remained in the entire country. Because of this there was not only a paucity of physicians to care for patients, but a severe shortage of medical educators to help train the next generation of physicians. A significant goal of the mission trip is to bridge this gap by providing lectures, conducting one-on-one teaching, and operating side-by-side with Cambodian medical students and physicians. The mission’s goal is to enable them to safely and confidently perform such procedures independently over time.
the Cambodian medical schools. After the reign of the Khmer Rouge ended in 1979, only 29 physicians remained in the entire country. Because of this there was not only a paucity of physicians to care for patients, but a severe shortage of medical educators to help train the next generation of physicians. A significant goal of the mission trip is to bridge this gap by providing lectures, conducting one-on-one teaching, and operating side-by-side with Cambodian medical students and physicians. The mission’s goal is to enable them to safely and confidently perform such procedures independently over time.
The annual mission to Cambodia is truly one of the highlights of the year for all involved. Patients come from all over Cambodia and sometimes wait for days to be evaluated for a potential surgery. The Soviet Friendship Hospital becomes their home while they wait for their operations and recover before starting the journey home. Historically, the mission has been completed once per year, but the number of patients presenting for evaluation continues to rise. Northwest Medical Volunteers, therefore, hopes to increase the frequency of their trips to Cambodia in the future to further offset the reconstructive needs of the Khmer people.
In May 2020 I traveled with the New York University (NYU) Department of Otolaryngology to Ulaanbaatar, Mongolia, for a humanitarian mission.
Zahrah M. Taufique, MD
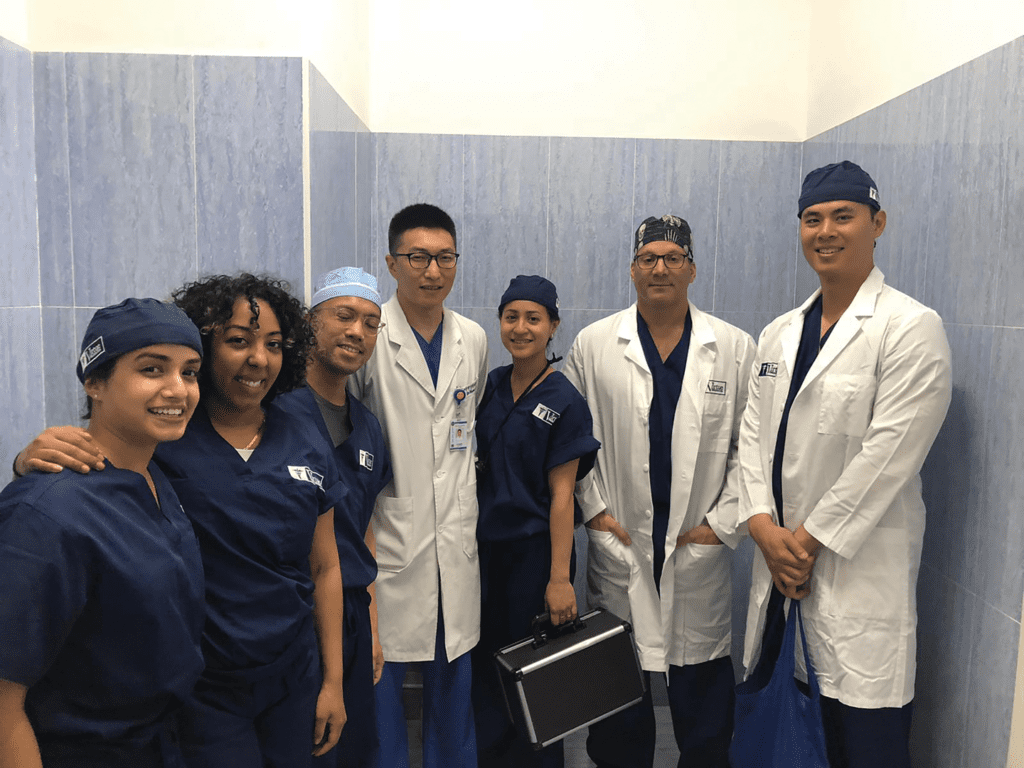
In May 2020 I traveled with the New York University (NYU) Department of Otolaryngology to Ulaanbaatar, Mongolia, for a humanitarian mission. The surgical team was composed of head and neck surgeons Theresa Tuyet-Phuong N. Tran, MD, and Adam S. Jacobson, MD, along with me, a fourth-year resident, and microvascular fellow Jason L. Yu, MD. We were accompanied by physician assistant Sabrina Tarafdar, as well as operating room nurses Ana Mae Gaolingo, Justine Padilla, Chris Abanico, Vicsyl Rodriguez, and Lauren Hamill.
Mongolia is an East Asian country that lies between China and Russia. The Mongolian Empire was the largest empire to have ever existed due to the leadership of Chinggis Khan, a figure who still heavily dominates current Mongolian culture. As a result of its historically nomadic culture, its capital Ulaanbaatar only settled in its current location in 1773. The group traveled with the Virtue Foundation, a nonprofit organization that has been sending surgeons to Mongolia for over a decade.
There were two hospitals in Ulaanbaatar where the group attended clinic and operated: the military hospital and the National Cancer Center. Though team members performed a variety of surgeries ranging from rhinoplasties to oncologic resections, they discovered there was a great need for education on reconstructive techniques for oncologic, traumatic, and iatrogenic defects. Specifically, microvascular reconstruction is a relatively new field in Mongolia. The only hospital in Mongolia currently performing free flaps is the National Cancer Center, where the first free flap was performed about 10 years ago. Still, the demand for free flap reconstructive expertise is high, and the surgeons performing these surgeries were eager to learn from the NYU group throughout the week.
One exemplary case was a fibular free flap for an orocutaneous fistula in a young man who had suffered from a gunshot wound to the face one year prior. He had undergone mandibular plating immediately after the injury; however, there was nonunion of the bone and fistula development. He had been following up at the military hospital for some time for local wound care. Upon arrival in Ulaanbaatar, the NYU team reviewed his case, and he underwent segmental mandibulectomy, excision of orocutaneous fistula, tracheostomy, fibula free flap, and plating. His postoperative course was uneventful. He was decannulated on postoperative day four and was able to resume a diet one week after surgery. Though the surgery itself was a success, even more valuable was the ability to teach the local surgeons these techniques and improve on their baseline knowledge of head and neck surgery.
By the end of the week, it was clear that a strong partnership developed between the American and local surgical teams, and there is ongoing discussion on how to continue this educational relationship in the future.
For the past 20 years, teams of otolaryngologists have provided continuous cleft care for patients in Kijabe, Kenya, through Samaritan’s Purse World Medical Mission and partnering with IAC-CURE Children’s Hospital and Smile Train.
Heather A. Koehn, MD
For the past 20 years, teams of otolaryngologists have provided continuous cleft care  for patients in Kijabe, Kenya, through Samaritan’s Purse World Medical Mission and partnering with IAC-CURE Children’s Hospital and Smile Train. Our team of physicians consisted of Lisa M. Buckmiller, MD (pediatric otolaryngology, San Antonio, Texas), Charles W. Ford, MD (otolaryngology-head and neck surgery, Boone, North Carolina), John J. Christophel, MD, MPH (otolaryngology-head and neck surgery, Charlottesville, Virginia), Patrick D. Munson, MD, (pediatric otolaryngology, Sioux Falls, South Dakota), Ryan H. Belcher, MD (pediatric otolaryngology, Nashville, Tennessee), and Ashley D. Baracz, MD (pediatric anesthesiology, San Antonio, Texas).
for patients in Kijabe, Kenya, through Samaritan’s Purse World Medical Mission and partnering with IAC-CURE Children’s Hospital and Smile Train. Our team of physicians consisted of Lisa M. Buckmiller, MD (pediatric otolaryngology, San Antonio, Texas), Charles W. Ford, MD (otolaryngology-head and neck surgery, Boone, North Carolina), John J. Christophel, MD, MPH (otolaryngology-head and neck surgery, Charlottesville, Virginia), Patrick D. Munson, MD, (pediatric otolaryngology, Sioux Falls, South Dakota), Ryan H. Belcher, MD (pediatric otolaryngology, Nashville, Tennessee), and Ashley D. Baracz, MD (pediatric anesthesiology, San Antonio, Texas).
With the support of the AAO-HNSF Humanitarian Travel Grant, I was able to serve with this team of talented surgeons and compassionate caregivers. It is humbling to see how a short surgery can provide such a profound difference in a patient’s life. Of the 72 surgeries that were performed over five days, one patient’s story will not be forgotten. Jackline is a 22-year-old mother of three who traveled to Kijabe from a rural Maasai village. She was brought by a local missionary who heard of our team’s visit to provide cleft surgery free of charge. She was born with a bilateral cleft lip and palate. She existed in her community, constantly keeping her lower face covered because of the deformity. She was the only person in her village with a cleft. Once arriving at the AIC-CURE Children’s Hospital campus, she saw the many children with clefts and immediately felt a sense of community and trust and uncovered her face. She underwent bilateral cleft lip surgery with our team. Two days later she left the hospital with a big smile and no covering on her face. She is pictured with her three-month-old baby and friend from her village as well as her surgeon team, Dr. Christophel, and me.
There is a lasting impression of this opportunity to provide cleft care as an otolaryngologist internationally. As a future pediatric otolaryngologist, I hope to establish a long-term service relationship like the team I was privileged to join and inspire others to do the same.
